The USMLE Step 2 Step Prep
ACT & SAT Test Prep for 2025 One-on-one test prep for ACT & SAT
MCAT prep begins now! MCAT prep for 2025
Bridging the Gap (Year) Career Coaching
Professionalism & Early-Career Physicians
Interview with LAS Founder, Loren Deutsch
LAS is seeing increases in referrals from GME departments and self-referred individuals for professionalism, among early-career physicians. The increase is concerning and with many factors contributing to professionalism (e.g., personal, academic, and more), this increase has informed many of the LAS Team Meetings, becoming a topic that leads to further inquiry and training.
The first question we ask a new client is, “How are you doing?”, the next is to clarify the professionalism issue, “Do you have a Professional Improvement Plan (PIP) or Remediation Plan?”, and the third involves the LAS Team and focuses on questions about Milestones and core competencies associated with professionalism, “Which ACGME Milestones and Competencies are implicated?”.
In most cases, the answers to these questions include, “Terrible”, “Yes”, and “I don’t know”. The “I don’t know” answers quickly become part of a spreadsheet whereby we identify the Milestones and Competencies for the Resident and our Team to develop incremental goals for a PIP. These goals become part of an ongoing discussion with the Resident, a Mentor, and the Program Director.
In most cases, the answers to these questions include, “Terrible”, “Yes”, and “I don’t know”. The “I don’t know” answers quickly become part of a spreadsheet whereby we identify the Milestones and Competencies for the Resident and our Team to develop incremental goals for a PIP. These goals become part of an ongoing discussion with the Resident, a Mentor, and the Program Director. As one of our Residents explained, being cited for professionalism problems felt like “a gut punch” and as the subreddit below indicates, it’s “a wakeup call”. To better understand what we’re seeing at LAS,
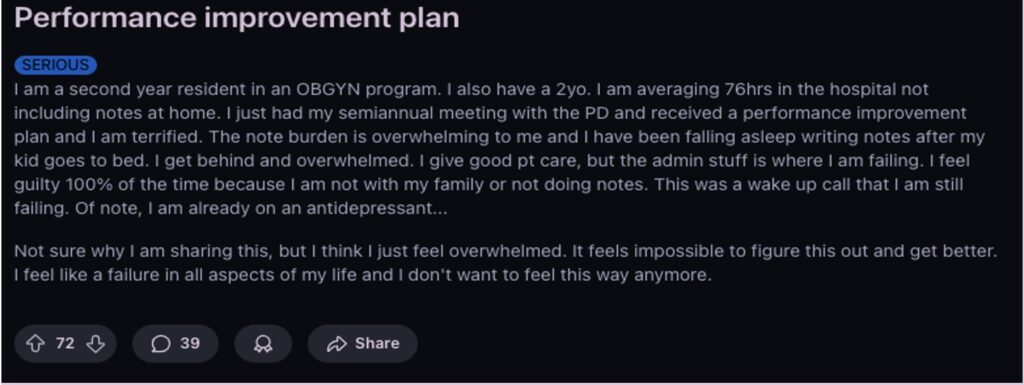
Professional Improvement Plan (PIP) from Reddit
How would you define professionalism in medicine?
“Regarding medicine and healthcare, I think professionalism speaks to patient safety, quality of healthcare, interactions with the patient and family, and the communication or direct involvement with other healthcare and administrative professionals in the work setting (e.g., hospital, clinic, or private office). The Accreditation Council for Graduate Medical Education (ACGME) requires early-career physicians to develop skills associated with professionalism, including communication, documentation, and coordinated work in graduate medical education. Professionalism is one of six core competencies required in medical training”.
What are some of the main reasons that you see for creating a performance plan?
“Lately, I am seeing PIPs that emphasize professionalism, with concerns associated with safety and quality patient care. These factors are associated with medical knowledge, medical skills, interpersonal communication, documentation, and inquiry, among others. When a Resident progresses through training, their responsibilities increase, and inherent to that, Residents are expected to perform them safely, accurately, and at an independent level. Despite many protective layers in training programs, designed to ensure safety and quality healthcare, PIPs seem concerned with whether a Resident can advance given a program’s support framework and timeframe”.
What are some factors that negatively impact professionalism in training programs?
“There are many factors that impact professionalism in training programs, positively, negatively, and sometimes both. Some of the most prevalent include high acuity rates, competing demands for time, vague or unclear feedback, and burnout, among others. However, it appears that internal communication is a common thread. I think these factors are opportunities for designing consistent protocols relative to training, feedback, and follow-up”.
How do PIPs get resolved? What are the next steps?
“To begin, we conduct an initial consultation with the Resident (like an “H + P” without the “P”). In follow-up, we design and co-create an individual plan with measurable goals and a shared spreadsheet for daily workflow, actionable steps, self-reflective processes, and progress tracking. These resources are shared with the Resident and are a key component of weekly, online coaching sessions and plan success. With the Resident’s consent, I also recommend meeting as a group, with the Resident and GME department (e.g., Resident, Program Director, Coordinator, and Mentor) to set expectations and confirm the timeline. My goal is to engage all stakeholders, support the Resident, and discuss how to realistically implement the actionable steps needed to address the PIP so the Resident fulfills the requirements. This last step is critical”.
What general advice do you have for Residents with a PIP?
“It’s important to recognize the seriousness of a PIP. It is a legal document and has implications for one’s professional development and medical career. I also encourage Residents to organize all written feedback from their program as it pertains to a PIP and confirm all deadlines and topics detailed in the PIP document. Next, I suggest contacting a mentor within the department to schedule regular meetings (weekly, bi-weekly, etc.) that can be used for feedback, practice, progress, etc., and select an outside coach to develop the actionable steps needed to fulfill the PIP and provide structure, support, and accountability”.
Professionalism, ACGME Milestones, and LAS Medical Coaching
 Professionalism: National Report Findings 2016
Professionalism: National Report Findings 2016
ACGME Common Program Requirements
LAS Consulting Services and LAS Medical Coaching
Leadership: A Fundamental Yet Undervalued Skill in Healthcare, HMS

